covid case
CASE PRESENTATION
A 38-year-old male who is a cycle mechanic by occupation presented to the OPD on 6/6/2021 with the
chief complaints of
- high-grade fever since 5 days
- generalized body pains since 4 days
- chest pain since 4 days
The patient was apparently asymptomatic 5 days back, Later he developed a fever of high grade not reliving with medication since 5 days, backache and joint pains since 4 days and he tested for SARS-COV-2 where the result turned out to be negative. Later, an investigation of chest pain got HRCT CHEST done which showed CORADS 5.
On 8/6/21 patient complained of severe headche, with left sided earache,facial pain and tooth ache. So patient was referred to the ent and dental department for opinion
He had no nasal obstruction, nasal discharge, nasal bleed and no anosmia
No c/o of cough, hemoptysis, SOB
History of past illness:
- known case of diabetes mellitus type II
- no h/o previous hospitalization
- no HTN, Asthma, TB, CAD
- no history of any previous surgeries
Tab METFORMIN -1000Mg/OD
TAB GLIMEPERIDE-2Mg/OD for DM TYPE II for 1 year.
other medications; for covid 19, TAB FAVIPIRAVIR -1600Mg /stat dose taken.
Personal History:
Married
Appetite -normal
sleep: adequate
Diet; Mixed diet
Bowel and bladder movements: regular
micturition :normal
no known allergies
addictions: regular gutka chewer
Family History: No significant family history
GENERAL EXAMINATION:
The patient is conscious, coherent, cooperative, well-nourished, well -oriented to time, place, person,
Pallor: no
Icterus: no
Cyanosis: no
Lymphadenopathy: no
Edema: no
Clubbing of fingers: no
VITALS at the time of admission: (4pm)
Temperature: 100 F (febrile)
Pulse rate: 99/min
On 8/6/21 PR: 48/min
Respiration rate :33 cycles/min
BP : 100/60 mm/hg
SPO2 at room air: 78%
92% on 15 lit of O2
On 8/6/21 spo2 : 94% on 12 lit of O2
GRBS: 262 mg%
SYSTEMIC EXAMINATION
CVS: S1 & S2 heard
no murmurs and cardiac thrills
RESPIRATORY SYSTEM:
Dyspnoea: present
Wheeze: absent
no adventitious sounds heard
ABDOMEN:
Inspection
the shape of the abdomen: scaphoid
palpation;
Tenderness- not present
no palpable mass
hernial orifices: normal
liver and spleen not palpable
percussion :
liver span: normal
auscultation;
bowel sounds: yes
CNS: intact
gait: normal
ENT :
It was done on day 8 of illness.
External frame work-normal
columella and vestibule -normal
septum -Centre
mucosa-normal
turbinates-normal
PNS -normal
oral cavity- normal
teeth-nicotine stained
Oropharynx-normal.
DENTAL examination
Malpositioned
Lingual mucosa and patient has Tenderness on palpation
tooth is tender on percussion
Oral swelling at angle of mandible extending till zygomatic arch.
INVESTIGATIONS
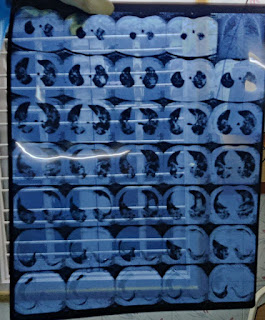
HRCT -CHEST scan
CORADS -5
CT SCORE - 22/25
RFT :
uric acid : 3.3 mg/dl
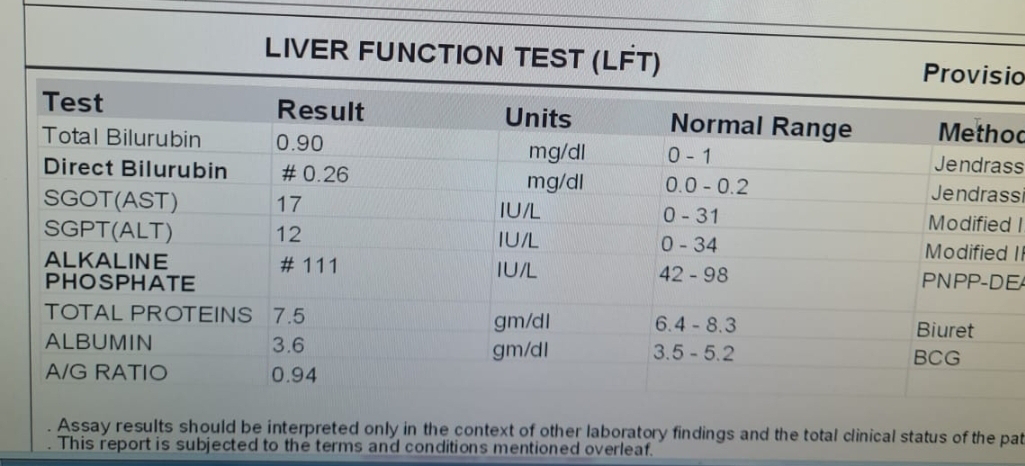
LFT:
total bilirubin: 1.79 mg/dl
direct bilirubin: 0.33 mg/dl
SGOT;47 IU/L
SGPT : 54 IU/L
ALKALINE PHOSPHATE: 207 IU/L
TOTAL PROTEINS: 5.9 gm/dl
ABG:
AFTAB ABG :9 PM
ph: 7.33
pco2: 40.4
po2: 39.3
saturation: 62.6%
bicarb :21.2
standard bicarb : 20.5
CBP;
Hb-13.2%
TLC-6900/mm3
platelet count-1.71 lacs
CRP +VE
ECG:
Provisional Diagnosis :
viral pneumonia secondary to COVID 19 and left lower tooth apical abscess and buccal space infection.
Treatment history:
on 6/6/21 (4pm)
1) O2 supplementation -15 lit/min maintain spo2>90%
2) intermittent BiPap
3)inj. dexamethasone -6mg i.v /od
4) inj. clexane- 40mg s.c / od
5) tab Limcee -po/tid
6) tab : zincovit PO/OD
7) inj. HAI- S.C ss after informing p.g ( 8 am -1pm-8pm)
8) GRBS monitoring -8th hrly (8-1-8-2)
9) tab dolo -650 mg PO/ tid
10) tepid sponging /ice packs
11) fever charting 4 hrly
12)monitor vitals
13) inj. Remedesivir -200mg i.v stat
100mg i.v OD for 5 days