covid case
CASE PRESENTATION
A 38-year-old male who is a cycle mechanic by occupation presented to the OPD on 6/6/2021 with the
chief complaints of
- high-grade fever since 5 days
- generalized body pains since 4 days
- chest pain since 4 days
The patient was apparently asymptomatic 5 days back, Later he developed a fever of high grade not reliving with medication since 5 days, backache and joint pains since 4 days and he tested for SARS-COV-2 where the result turned out to be negative. Later, an investigation of chest pain got HRCT CHEST done which showed CORADS 5.
No c/o of cough, hemoptysis, SOB
History of past illness:
- known case of diabetes mellitus type II
- no h/o previous hospitalization
- no HTN, Asthma, TB, CAD
- no history of any previous surgeries
Tab METFORMIN -1000Mg/OD
TAB GLIMEPERIDE-2Mg/OD for DM TYPE II for 1 year.
other medications; for covid 19, TAB FAVIPIRAVIR -1600Mg /stat dose taken.
Personal History:
Married
Appetite -normal
sleep: adequate
Diet; Mixed diet
Bowel and bladder movements: regular
micturition :normal
no known allergies
addictions: regular gutka chewer
Family History: No significant family history
GENERAL EXAMINATION:
The patient is conscious, coherent, cooperative, well-nourished, well -oriented to time, place, person,
Pallor: no
Icterus: no
Cyanosis: no
Lymphadenopathy: no
Edema: no
Clubbing of fingers: no
VITALS at the time of admission: (4pm)
Temperature: 100 F (febrile)
Pulse rate: 99/min
Respiration rate :33 cycles/min
BP : 100/60 mm/hg
SPO2 at room air: 78%
92% on 15 lit of O2
GRBS: 262 mg%
SYSTEMIC EXAMINATION
CVS: S1 & S2 heard
no murmurs and cardiac thrills
RESPIRATORY SYSTEM:
Dyspnoea: present
Wheeze: absent
no adventitious sounds heard
ABDOMEN:
Inspection
the shape of the abdomen: scaphoid
palpation;
Tenderness- not present
no palpable mass
hernial orifices: normal
liver and spleen not palpable
percussion :
liver span: normal
auscultation;
bowel sounds: yes
CNS: intact
gait: normal
INVESTIGATIONS
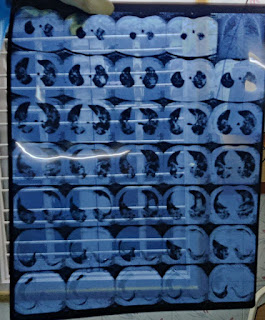
HRCT -CHEST scan
CORADS -5
CT SCORE - 22/25
RFT :
uric acid : 3.3 mg/dl
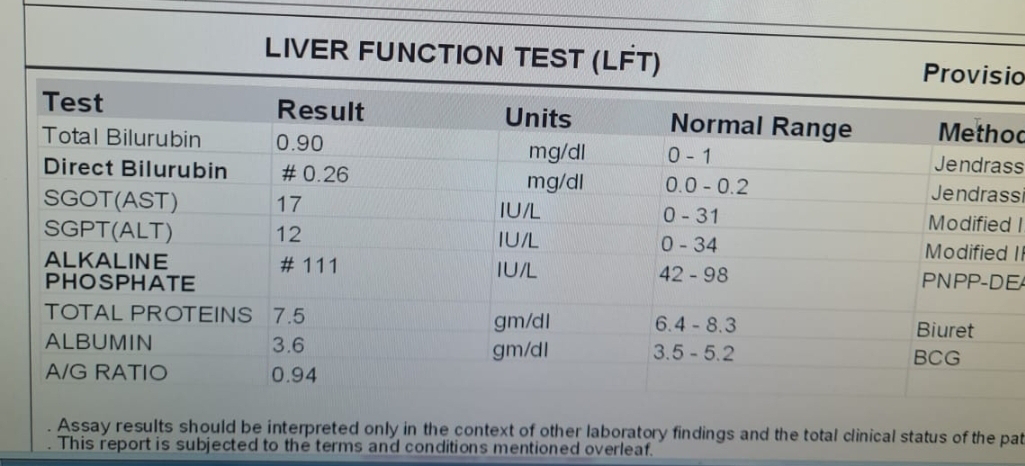
LFT:
total bilirubin: 1.79 mg/dl
direct bilirubin: 0.33 mg/dl
SGOT;47 IU/L
SGPT : 54 IU/L
ALKALINE PHOSPHATE: 207 IU/L
TOTAL PROTEINS: 5.9 gm/dl
ABG:
AFTAB ABG :9 PM
ph: 7.33
pco2: 40.4
po2: 39.3
saturation: 62.6%
bicarb :21.2
standard bicarb : 20.5
CBP;
Hb-13.2%
TLC-6900/mm3
platelet count-1.71 lacs
CRP +VE
ECG:

Provisional Diagnosis :
viral pneumonia secondary to COVID 19
Treatment Given:
on 6/6/21 (4pm)
1) O2 supplementation -15 lit/min maintain spo2>90%
2) intermittent BiPap
3)inj. dexamethasone -6mg i.v /od
4) inj. clexane- 40mg s.c / od
5) tab Limcee -po/tid
6) tab : zincovit PO/OD
7) inj. HAI- S.C ss after informing p.g ( 8 am -1pm-8pm)
8) GRBS monitoring -8th hrly (8-1-8-2)
9) tab dolo -650 mg PO/ tid
10) tepid sponging /ice packs
11) fever charting 4 hrly
12)monitor vitals
13) inj. Remedesivir -200mg i.v stat
100mg i.v OD for 5 days